The landscape of prenatal testing is confusing, partly because its evolution has been so rapid. When I was pregnant the first time, which was both a long time ago and not that long ago, there were ultrasound-based screening procedures and invasive tests. When I was pregnant the second time, cell-free fetal DNA testing had been added. Since then, that testing has improved, the set of conditions it can screen for has improved, and on and on. It can be quite difficult to figure out how, exactly, these all fit together.
Here’s an example question from the mailbox:
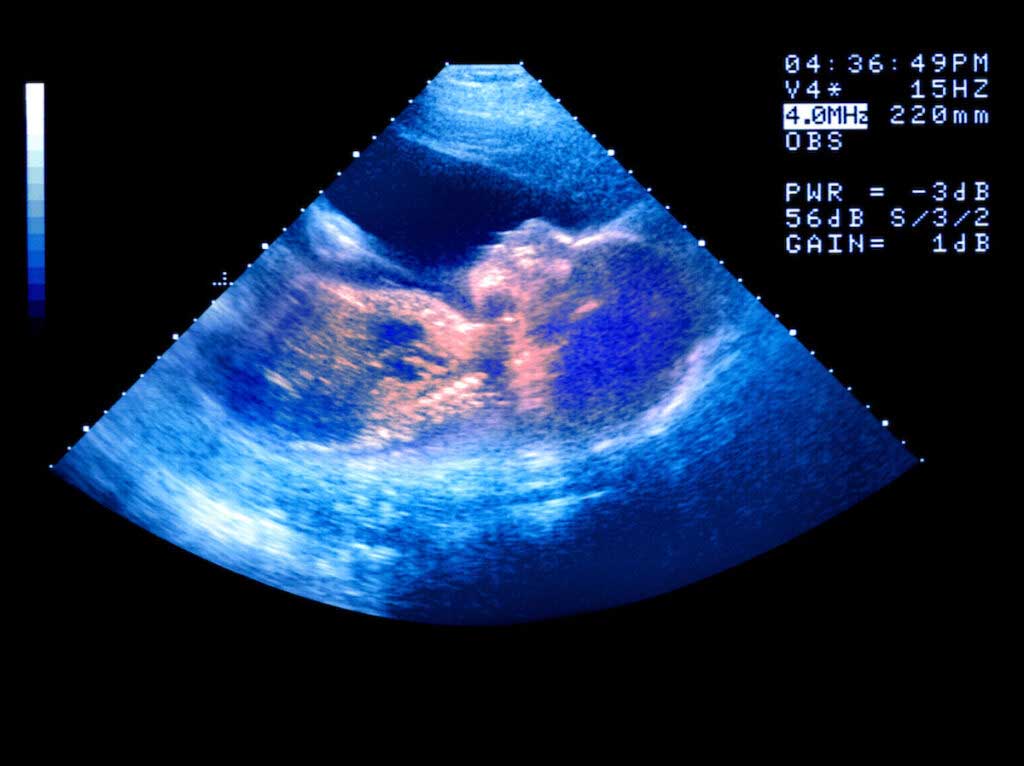
I just had my 19-week ultrasound, and the doctor told me our baby has dilated renal pelvis (4.9 millimeters, which is over the standard max. of 4mm). Even though my cell-free DNA test came back as negative for trisomy 21, they said the chance our baby has Down syndrome has increased from 1 in 10,000 to 1 in 5,200. In the end, dilated renal pelvis is pretty common. Any insight on your end as to how worried we should be that our baby has Down syndrome? I want to avoid invasive testing if at all possible.
This person has had two tests — a cell-free screening and an ultrasound. How do they combine? How should they be combined? Is invasive testing necessary? Where do these numbers even come from?
Today we’ll dive into a review of this testing. The space is big, so we’re going to limit the scope. I’m going to focus on testing for the three most common trisomies (genetic conditions in which there is an extra, third, copy of a chromosome) — trisomy 21, 18, and 13. I’ve written before about the expansion of cell-free testing to other conditions, here. I’ll talk through the various ways these can be detected, the accuracy rates, and how it all gets put together. (There is a little bit of TL;DR at the end, if you want to skip down.)
Testing options
Cell-free fetal DNA testing
Cell-free fetal DNA testing began to be used in the mid-2010s. These tests make use of the fact that some fetal DNA circulates in the maternal bloodstream. Treated correctly, a sample of blood from the pregnant person can be used to detect abnormalities in the fetus. To somewhat simplify, the approach is to look for evidence of DNA that wouldn’t otherwise be in the mother.
For example: Let’s say you wanted to know the baby’s sex. The pregnant person typically has two X chromosomes. A male baby will have an XY, and a female will have XX. If you sample mom’s blood and find evidence of circulating Y chromosomes in the cell-free DNA, this indicates a male fetus (since the mom’s own cell-free DNA wouldn’t contain a Y chromosome).
These tests can be used to detect an infant’s sex and the three primary trisomies (Down syndrome, trisomy 13, and trisomy 18). Detecting a trisomy means, effectively, looking for an imbalance in the presence of these chromosomes in the cell-free DNA. Assuming the pregnant person has two copies of each chromosome, if you observe an excess of chromosome 21 in the cell-free DNA, it suggests this must be due to an excess of chromosome 21 in the fetus, which would suggest Down syndrome.
Cell-free testing relies on a maternal blood sample, typically taken at around 10 or 11 weeks of pregnancy (testing too early can lead to inconclusive results, since the amount of fetal DNA increases over time).
These tests are extremely accurate. Based on a 2017 meta-analysis, cell-free testing would detect 99.4% of trisomy 21 cases, 97.7% of trisomy 18 cases, and 90.6% of trisomy 13 cases. The false-positive rates are also quite low — 0.1% for all three. Because these conditions are rare, even these relatively small false-positive rates mean that a reasonable share of positive tests are false positives, but the overall performance of the test is excellent. In particular, an enormous share of the cases of these three conditions are detected based on these tests.
Invasive testing: amniocentesis and CVS tests
There are two approaches to invasive prenatal testing: amniocentesis, where a sample of amniotic fluid is used for testing, and chorionic villus sampling (CVS), in which a sample is taken from the placenta.
In either of these cases, the accuracy of the tests performed is close to 100%. Because you are directly sampling DNA, it is possible to actually look directly at the chromosomal makeup. These tests can also be used for other conditions beyond trisomies, since you can look at the full set of chromosomes.
The main concern with invasive testing is possible risks to the fetus, notably miscarriage. Women are often quoted procedure-related miscarriage risks of 1 in 100 or 1 in 200. These are overestimates. A 2019 review suggests that when an appropriate control group is used, neither amniocentesis nor CVS is associated with a significantly higher miscarriage risk (and the point estimates are very small or negative).
Because these are invasive procedures, it is hard to say they have no risk at all, but in the data their risks seem to be negligible.
PGT
If you got pregnant through IVF, you may have done preimplantaion genetic testing (PGT). Similar to the invasive testing options, this is close to 100% accurate for these trisomies (it can be wrong in very rare cases).
Other ultrasound and blood-test-based screenings
There are a number of ultrasound-based tests that can be used as a screen for trisomies. The best-known one is NT (nuchal translucency) testing. At around 12 weeks, an ultrasound can take a measurement of fluid behind the neck. Fetuses with trisomy 21 are more likely to have more fluid behind the neck. A high reading on this test therefore suggests a higher risk of the fetus being affected. This is typically combined with a blood test, which has some screening value. The measurements are also combined with individual age. All together, they generate a risk value based on the screening and people either “screen positive” (meaning they are above some risk cutoff) or “screen negative” (meaning they are below).
These tests are substantially less accurate than cell-free fetal DNA testing. The NT + blood testing would detect perhaps 80% of cases, depending on maternal age, with a high false-positive rate (about 4% on average). The reason for this is fairly simple — although fetuses with trisomy 21 are more likely to have a large amount of fluid, a lot of other babies do too. This is just not a super-accurate marker.
There are a large number of markers like this. There are results from blood tests and ultrasound findings that are more common when a fetus has a trisomy. It’s important to note, though, that these all have fairly weak predictive power. None of them comes anywhere close in accuracy to the cell-free options, which is why they are increasingly less used.
Combining metrics
Given this option set, we can think about what we learn at any given stage of testing. Big picture:
- Each new piece of information helps us learn something, but how much we learn depends on what we thought before.
- We need Bayes’ rule.
This is perhaps best illustrated by going back to a version of the question we started with. Let’s say at your 20-week ultrasound, there is evidence of a “soft marker” (a finding that may indicate an increased risk) for Down syndrome. How much do we learn from that? The answer depends tremendously on what you knew before.
Scenario 1: You’ve done PGT or some type of invasive testing, and it is negative
If you have a full DNA test from your fetus, the chance that they have trisomy 21 is essentially zero. The soft marker that you observe on the ultrasound is something that occurs in some babies with normal chromosomes and at higher rates in babies with Down syndrome. However, since you know your baby has a normal set of chromosomes, there is nothing to learn here. The chance is still essentially zero.
Scenario 2: You have a cell-free fetal DNA test, and it is negative
The cell-free testing detects a huge share of Down syndrome cases, but not all. Therefore, the risk is not zero. So we need some numbers.
Beginning at the beginning: Based on maternal age, there is some baseline risk of Down syndrome. Let’s assume it’s 1 in 500. The cell-free fetal DNA test detects 99.4% of cases. This means that after a negative test, the remaining chance is 0.006 per 500, or about 1 in 83,333.
Now we imagine you’ve got a soft marker signal on ultrasound — to be specific, let’s go with dilated renal pelvis. This is a condition that appears in about 17% of fetuses with Down syndrome and about 2.5% of fetuses without it. This information, together with the baseline risk, is enough to make a calculation of the chance that your fetus has Down syndrome given a positive test. This calculation relies on Bayes’ rule; there are more details on this in the post linked above. But the overall concept involves taking the baseline risk and adjusting based on the value of the new information.
With this new information, the risk is increased from 1 in 83,333 to 1 in 12,255. This is higher, but it is still extremely small. It’s an increase from 0.0012% to 0.0081%. These numbers are both tiny.
Scenario 3: You have no testing before
A third possibility is that you encounter one of these soft markers without any prior information.
We can continue with the dilated renal pelvis example. We imagine now that there was no testing done before, so the starting risk is 1 in 500 (your basic, baseline risk). With a positive test — applying Bayes’ rule — the updated risk is 1 in 74. This is still a very small number but much higher. And the actual increase in risk is much bigger in this case than in the prior one.
There is no really correct answer as to how to combine these tests, because so much of the right choice depends on individual preference. Faced with scenario 2, some people would choose to get an invasive test to be sure. Others will not.
There is, I think, an interesting question about whether these soft markers are useful at this point if someone has already had cell-free fetal DNA testing. On one hand, they do provide some additional information. On the other hand, I suspect it will rarely be the case that this information will be enough to push someone into more invasive testing.
Bottom line
- If you want to be sure about trisomy detection, either amniocentesis or CVS testing is necessary. These carry minimal risks.
- Cell-free fetal DNA testing is extremely accurate for detecting the primary trisomies (21, 13, 18). Although there are a small number of false negatives, it is very rare.
- Ultrasound findings rarely provide much information if you’ve already had cell-free fetal DNA testing, and no additional information if you have had invasive testing.