Why are there so many prenatal appointments in the third trimester? Are all of them really necessary? I’m at 33 weeks, and of course, I want to do what is evidence-based, but I feel like I need to move my life around to make it to every single visit.
— Is This Extra?
It’s been a while, but I distinctly remember this same feeling when I was in your shoes. There was one appointment — at 38 weeks — where my doctor was running 90 minutes behind. I wondered: How important is this appointment, really? Should I just leave? On the other hand, I wanted the best care, and prenatal care guidelines are presumably put there for a reason.
This question — how valuable is medical care — comes up all the time in medicine, and especially in preventative care, which is what most prenatal care really is. You’re trying to make sure everything is going well. Most of the time, it is, and the appointment was not necessary. This leads to the question of whether maybe fewer appointments would be fine.
How valuable is the marginal visit to your doctor or the marginal ultrasound? If doctors saw low-risk people less frequently in their last months of pregnancy or did fewer tests, would it matter very much?
These questions matter for medical professionals and patients, but they are hard to answer. Choices about the amount of care that individuals receive will depend on their other characteristics. People who get more ultrasounds during pregnancy tend to have more complications, but that’s not because the ultrasounds cause complications; it’s because the complications cause the need for ultrasounds.
Answering this question reliably requires finding a source of variation in prenatal care that is more random. A 2021 paper in JAMA Health Forum does this using a technique called “regression discontinuity.”
Here’s the idea.
In the U.S., women who are over 35 on their due date are classified as “advanced maternal age,” or AMA. People in this category are given more screening and testing, and more prenatal care in general. This reflects the fact that, on average, older ages bring more complications. Importantly, though, there is nothing special from a biological standpoint about turning 35.
People who are due to give birth at 34 years and 364 days are not at higher risk, on average, than those due at 35 years and 1 day. But, because of insurance rules, the person who will be 35 and 1 day can expect to have more prenatal screening and testing. The core method in this paper is to look at whether these extra services lead to better outcomes.
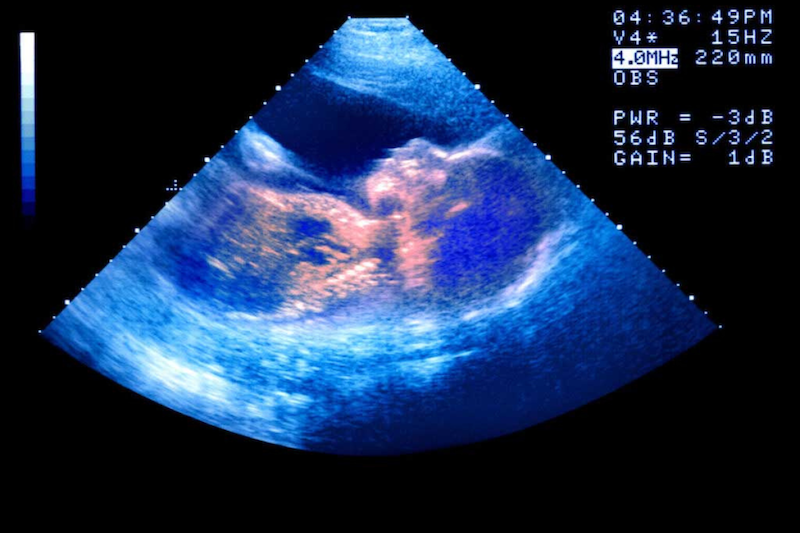
The researchers show first that women over 35 are more likely to have more advanced prenatal care. The most striking graph is on detailed ultrasound scans; I’ve included it below. It is pretty clear from this picture that when you tick over that age-35 cutoff (the x-axis of this graph is denoted in days around the 35th birthday), you get more scans.
The paper then goes on to look at whether this extra screening matters for mothers and infants. The authors find no impact on severe complications for mothers, but they do find a significant decline in stillbirth and early neonatal death. This means there is a reduction in stillbirth as a result of the added monitoring. The reduction is about 0.4 percentage points; you can see this in the graph below. This is a large effect, about a 40% reduction from the baseline risk.
Overall, this finding suggests that the added monitoring and screening are having an important impact, at least in this population. What does this mean for you? It provides some evidence that the many prenatal visits you’re having may make a positive difference. Hang in there!
Community Guidelines






















Log in